
The QRS complex is wide due to ventricular depolarization proceeding outside the conduction system. Spontaneous atrial activity is sensed by the atrial lead and triggers ventricular stimulations. The ventricles are depolarized via the His-Purkinje network, resulting in normal QRS duration. Atrial pacing with normal conduction to the ventricles via the AV system. If the lead tip is fixed in the septum, the impulse may actually enter the conduction system (His-Purkinje network), which results in rapid impulse transmission and thus shorter QRS duration (as compared with apical pacing).īecause ventricular pacing results in abnormal depolarization, repolarization will also be abnormal, resulting in discordant ST-T segments (i.e the QRS complex and T-wave display opposite directions).īelow follows ECG tracings demonstrating these aspects. Stimulation in other regions of the ventricle may result in a different QRS morphology. As mentioned above, this is similar to the situation in left bundle branch block (LBBB), which explains why paced QRS complexes are similar to the QRS morphology during LBBB. Typically, the lead tip is fixed apically in the right ventricle activation starts in the right ventricle and spreads slowly to the left ventricle. QRS morphology also depends on where the pacing stimulus is delivered. If the atrial lead is placed distally in the atrium, activation may proceed in the opposite direction, which results in negative (retrograde) P-waves in lead II. Typically, the atrial lead is fixed next to the right atrial appendage, or atrial ceiling, which yields P-waves similar to those seen during normal sinus rhythm (i.e, positive P-wave in lead II). The appearance of the P-wave depends on where the atrial lead is fixed. An intrinsic heart rate faster than the base rate should inhibit the pacemaker. The base rate is virtually always >50 beats/min, meaning that any heart rate below 50 beats/min is most likely not paced. The base rate is usually set to 60 beats/min. The base rate is the lowest heart rate allowed by the pacemaker intrinsic cardiac activity below the base rate will trigger pacing. The depolarizing wave spreads outside the conduction system, which is considerably slower, as compared with impulse transmission within the conduction system (His-Purkinje network). This is explained by the fact that, as in LBBB, the left ventricle receives the depolarizing impulse from the right ventricle (where the pacemaker delivers the pulses). In addition to stimulation artifacts, ventricular pacing yields wide QRS complexes with LBBB morphology (i.e left bundle branch block appearance). Stimulation artifact (red arrows) in ventricular pacing. The latter yields a discrete stimulation artifact, which may be visible in one or a few leads.
The stimulation artifact is larger in unipolar pacing, as compared with bipolar pacing. Two artifacts are seen if both chambers are paced.
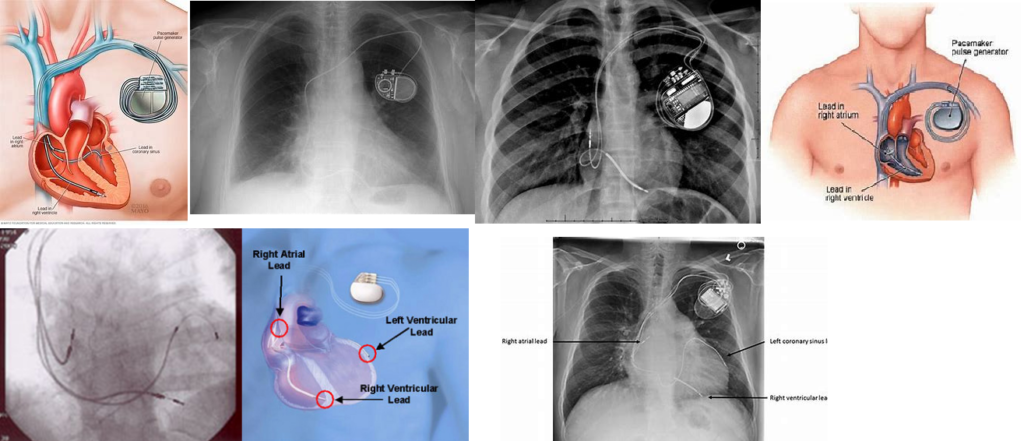
In ventricular pacing, the stimulation artifact precedes the QRS complex. In atrial pacing, the stimulation artifact precedes the P-wave. The cardinal manifestation of pacing on surface ECG is the stimulation artifact (Figure 1). Pacing activity may be visible or invisible, depending on e.g the type of pacemaker, intrinsic cardiac activity, etc. Being able to assess pacemaker function and perform troubleshooting should be considered a basic clinical skill. However, most clinicians who encounter patients with pacemakers only have access to conventional surface ECGs. Most modern devices are capable of transmitting ECG tracings continuously to cloud-based platforms, which enables the clinician to examine intracardiac ECGs at any time. Assessing pacemaker function requires knowledge of the mode of pacing, and careful analysis of ECG tracings.


 0 kommentar(er)
0 kommentar(er)
